Is the Carbohydrate-Insulin Model of obesity over?
Introduction
Obesity is ultimately the result of excessive body fat accumulation. Given the explosion of obesity rates around the globe, understanding how people become obese has been the center of much deserved scientific investigation. The consensus model that informs most attempts to prevent and treat obesity has to do with energy balance and the mismatch between caloric intake and expenditure [1]. As such, the overconsumption of highly palatable foods coupled with reduced physical activity (termed the ‘obesogenic environment’) leads to increased adiposity and poor health. Despite the wide acceptance of this model (often termed calories in, calories out or CICO), in recent years a new model has taken the nutrition research field by storm. This model also aims to explain the obesity epidemic given the lack of successful dietary preventatives and treatments for obesity based on the conventional model. The new model is termed the carbohydrate-insulin model (CIM) of obesity [2]. It posits that dietary carbohydrate, not energy balance, is the primary culprit. The guilt lay in carbohydrate’s ability to robustly increase insulin levels, thereby promoting fat storage and accumulation. This scenario, in turn, promotes increased dietary intake and further weight gain (see image comparing the models below; taken from Ref. 2).
While noble in its attempt, a number of popular diet books rely on the CIM in an effort to promote a low-carbohydrate/ketogenic style of eating—the latest being Gary Taubes’ most recent low-carbohydrate screed, ‘The Case for Keto’. If carbohydrate and insulin truly are the problem, then drive them as low as possible to prevent fat accumulation and promote health. Obesity epidemic solved! Or so the story goes [3]:
“By stimulating insulin secretion, carbohydrates make us fat and ultimately cause obesity. The fewer carbohydrates we consume, the leaner we will be.”
While the hypothesis is tempting (I guess), countervailing evidence suggests that this hypothesis is not correct [4-7]. (But who ever let a few pieces of opposing data ruin a good bias?) Which leads me to today’s (upcoming) article. The study we are about to examine explicitly set out to test the CIM and its predictions, plain and simple. If carbohydrate truly is the culprit, there should be a clear decrease in insulin levels, fat accumulation, and energy intake with a low-carbohydrate, ketogenic diet compared to another diet much higher in carbohydrate and lower in fat.
“Low-carb” and “keto”: a primer
Before getting to the paper, let us first define some terms and get ourselves oriented around what it means to eat “low-carb” and “keto.” In both situations, carbohydrate is reduced in the diet and is concomitantly replaced with higher amounts of fat (typically, protein goes up a bit as well given the types of foods allowed on the diet).
For some time, the term “low-carbohydrate” had no objective meaning, making it hard to compare across research studies using different levels of carbohydrate intake. Now, an objective definition exists for what low-carbohydrate actually means. A low-carbohydrate diet is one where less than 26% of your daily calories come from carbohydrate [8]. For the average 2,000-calorie diet, this equates to ~130 g per day. Obviously, if you have lower or higher caloric needs then this absolute amount will go up or down accordingly.
What about “keto”?
A ketogenic diet is a subcategory of a low-carbohydrate diet. As such, this style of eating reduces carb intake much more aggressively; typically well below 100 g per day (the importance of this will be explained shortly). For example, in the original installment of the Atkins Diet (which is a ketogenic diet), it recommended the consumption of just 20 g of carbohydrate per day. To help visualize how paltry this amount of carbohydrate is, a standard, medium-size banana contains roughly 27 g of carbohydrate. In the most recent version of Atkins, 50 g of carb per day is allowed. (How generous!)
As you can see, no matter how you slice it, if you are eating “low-carb” you are severely limiting your carbohydrate intake. In the study we will review shortly, carbohydrate intake in the low-carbohydrate group was well under 100 g per day, thus making it a ketogenic diet.
What is the significance of such a low carbohydrate intake?
By restricting carbohydrate intake to less than 100 g per day, this lowers insulin excursions and ultimately shifts your body’s metabolism to utilizing fat as a primary fuel source. This also allows the conversion of some of those fats to what are called ketones (or ketone bodies). This process takes place in the liver. For completeness, there are technically three types of ketones. They are beta-hydroxybutyrate (BHB), acetoacetate, and acetone. (Yes, the same acetone commonly found in nail polish remover.) Interesting fact: acetone is highly volatile (i.e. it evaporates) at room temperature, so individuals who have elevated levels of ketones in their body can give off a fruity/nail polish-y odor due to acetone on their breath. This is quite common in individuals with runaway diabetic ketoacidosis. (I digress.) Relating to the study I keep meaning to get to, blood levels of BHB were sufficiently elevated by one week on the low-carbohydrate diet, thus establishing it’s ketogenic bona fides.
The entire metabolic purpose of generating ketones is to provide your brain with a readily available fuel source when glucose is not available in sufficient amounts—e.g. during times of prolonged fasting/starvation or via reduced dietary carbohydrate intake. This is because under standard carbohydrate intake, your brain runs solely on glucose (~120 g per day) and does just well making a living this way. However, after a few days of low-carbohydrate intake, you exhaust your liver glycogen stores and your brain lacks the capacity to generate sufficient ATP from glucose derived from gluconeogenesis alone. Because it is incapable of using fats to generate energy (how unfortunate!), the brain relies on ketones to supply its remaining energy demands. (Pretty cool nonetheless!)
As such, a low-carbohydrate, ketogenic diet ultimately produces this shift in metabolism, which is commonly argued to confer fat burning superiority over diets higher in carbohydrate, thus leading to greater weight loss.
Now we return our attentions back to the CIM and the idea that carbohydrate causes obesity. By lowering dietary carbohydrate insulin will be lower, fat burning (and ketogenesis) will be higher, hunger will be reduced, and excess fat gain will be prevented. It was nice seeing you obesity!
Enter (finally) today’s study…
Effect of a plant-based, low-fat diet versus an animal-based, ketogenic diet on ad libitum energy intake [9]
This paper was published in the prestigious journal Nature Medicine and was a tightly controlled, inpatient crossover study where all participants—I repeat, all participants—received both dietary conditions for two weeks in random order. Thus, no explaining away the results due to individual differences between groups. (Sorry low-carb zealots, each person served as their own control and the consistency of their responses across the diets is, well, glorious. More on that later.)
Participants resided in the metabolic ward for the entire duration of the study, and any meetings between participants and outside visitors were conducted in a communal room under strict supervision by research staff. (No cheating here!)
All meals and snacks were meticulously calculated and provided to subjects on a seven-day rotating menu at defined times. Further, all meals between conditions were matched as close as possible for overall calories, protein, and non-starchy vegetables. The most important difference, aside from the animal and plant-based nature of the diets, was the relative contribution of calories from carbohydrates and fats (i.e. the only meaningful difference relevant to the CIM as stated), with the low-carbohydrate group receiving ~10% carbohydrate and ~75% fat and the low-fat group effectively reversed with ~10% fat and ~75% carbohydrate. It should also be mentioned that the glycemic loads of the diets were worlds away (i.e. 6 g vs. 85 g per 1,000 kcal in the low-carbohydrate and low-fat condition, respectively).
Thus, with that set up, were the CIM to be true, the low-fat group would secrete more insulin, store more fat, become increasingly hungrier, and consume vastly more calories, because, well, carbs. Conversely, the low-carbohydrate group would have lower insulin levels, lose more body fat, become less hungry, and consume fewer calories.
Study results
Drum roll, please…
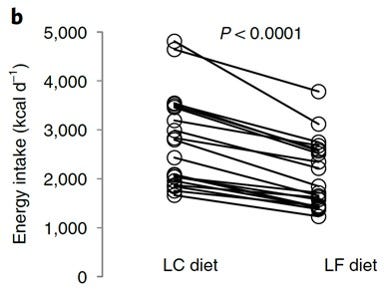
Despite a vastly higher carbohydrate intake, glycemic load, and higher postprandial insulin levels on the low-fat diet, not only did the low-fat condition not make the subjects hungrier, but the low-fat condition lead to significantly fewer calories consumed over the two-week period (~689 fewer calories per day) and lead to greater rates of fat loss (51 grams per day vs. 16.9 grams per day) compared to the low-carbohydrate condition. This is about as good of a refutation of the CIM as you can possibly get. The testable predictions just did not play out as put forth by the CIM.
And it’s not like the authors are hiding behind groups means with two individuals accounting for the overall differences. No, they also presented individual data. And the data is damning. As you can see below in what is probably the most condemning figure for the CIM in the manuscript: Every. Single. Person. Reduced. Their. Caloric. Intake. On. The. Low. Fat. Diet. I’ll let that sink in for a second. Not one person ate more on the low-fat diet. Not one. That’s like, zero people. Okay, I’m done.
Conclusions
Friendly sarcasm aside, this study is a gut punch to the CIM. Obvious limitations are the small sample size (n=20) and the ability to extrapolate to free-living conditions where “high carb” typically means high sugar coupled with high fat. Nevertheless, given the hypothesis of the CIM, as stated by those who promulgate it, the present study by Hall and company falsifies it outright.
So while it does not look like the low-carbohydrate diet is the savior of the obesity epidemic, I will finish with some compromising words, delivered by Hall himself, regarding the CIM and the low-carbohydrate diet (that I whole-heartedly endorse) [10]:
“It is important to emphasize that low carbohydrate diets may confer metabolic benefits beyond loss of weight and body fat regardless of whether or not the [CIM] is true or false. Furthermore, experimental falsification of important aspects of the [CIM] does not mean that dietary carbohydrates and insulin are unimportant for body fat regulation. Rather their role is more complicated than the [CIM] suggests.”
Until next time!
References
1. Schwartz, M.W., et al., Obesity Pathogenesis: An Endocrine Society Scientific Statement. Endocr Rev, 2017. 38(4): p. 267-296.
2. Ludwig, D.S. and C.B. Ebbeling, The Carbohydrate-Insulin Model of Obesity: Beyond "Calories In, Calories Out". JAMA Intern Med, 2018. 178(8): p. 1098-1103.
3. Taubes, G., Good calories, bad calories : challenging the conventional wisdom on diet, weight control, and disease. 1st ed. 2007, New York: Knopf. xxv, 601 p.
4. Hall, K.D., et al., Calorie for Calorie, Dietary Fat Restriction Results in More Body Fat Loss than Carbohydrate Restriction in People with Obesity. Cell Metab, 2015. 22(3): p. 427-36.
5. Hall, K.D., et al., Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men. Am J Clin Nutr, 2016. 104(2): p. 324-33.
6. Gardner, C.D., et al., Effect of Low-Fat vs Low-Carbohydrate Diet on 12-Month Weight Loss in Overweight Adults and the Association With Genotype Pattern or Insulin Secretion: The DIETFITS Randomized Clinical Trial. JAMA, 2018. 319(7): p. 667-679.
7. Hall, K.D. and J. Guo, Obesity Energetics: Body Weight Regulation and the Effects of Diet Composition. Gastroenterology, 2017. 152(7): p. 1718-1727 e3.
8. Oh, R., B. Gilani, and K.R. Uppaluri, Low Carbohydrate Diet, in StatPearls. 2020: Treasure Island (FL).
9. Hall, K.D., et al., Effect of a plant-based, low-fat diet versus an animal-based, ketogenic diet on ad libitum energy intake. Nat Med, 2021.
10. Hall, K.D., A review of the carbohydrate-insulin model of obesity. Eur J Clin Nutr, 2017. 71(5): p. 679.